Achilles Tendon Surgery
What is Achilles Tendon Surgery?
Achilles Tendon Surgeries are a group of procedures designed to resolve a number of Achilles Tendon problems and injuries.
The surgeries include:
- Repair - Direct repair of achilles tendon
- Debridement - Removal of damaged or degenerate tendon
- Tendon Transfer - If tendon has more than 50% damage
- Ostectomy - Removal of any bone spurs that are causing injury to the achilles tendon (e.g. Haglunds)
- Gastrocnemius recession
When is Achilles Tendon Surgery Indicated?
Achilles tendon surgery may be indicated for patients who have failed conservative therapies:
- Chronic tendon ruptures
- Tendinopathy
- Haglunds Deformity
Acute Achilles Tendon Rupture Surgery (Repair)
Traditionally it was thought that surgical treatment of acute ruptures resulted in a lower re-rupture rate. However, newer evidence shows that a functional rehabilitation program also has low re-rupture rates and avoids the complications of achilles surgery (such as wound complications and infection).
Therefore surgery is only indicated in:
- Late presentation ruptures (over 3 weeks)
- Chronic ruptures
Surgery for these cases can involve:
- Achilles Tendon Tear Repair
- Tendon Transfers: To help supplement the repair
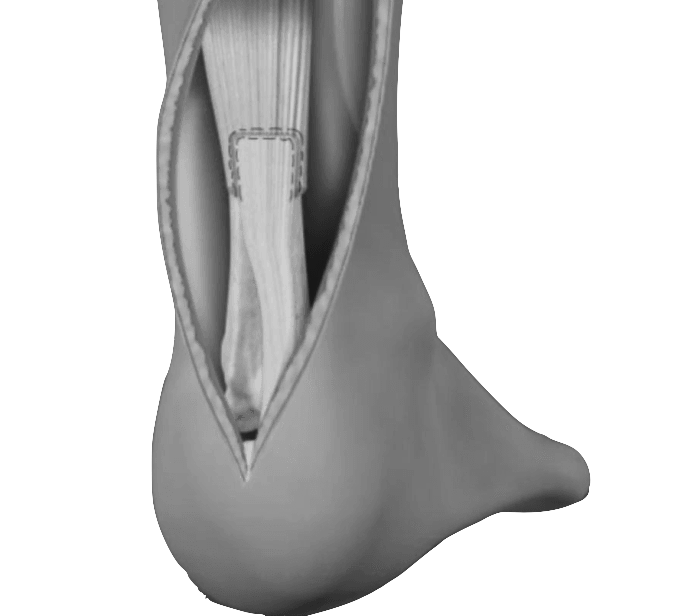
Debridement and Repair Surgery
Debridement and Repair may be suitable when less than 50% of the tendon is damaged. The damaged part of the Achilles tendon is removed, followed by tendon repaired with sutures, or stitches.
Debridement with Tendon Transfer Surgery
Debridement with Tendon Transfer may be suitable when more than 50% of the tendon is damaged. The damaged part of the Achilles tendon is removed, and if the remaining portion of the tendon is not strong enough to function alone an Achilles tendon transfer is performed. This additional tendon is used to supplement the repair. The extra tendon used is the tendon that helps the big toe point down. This is moved to the heel bone to add strength to the damaged tendon. The big toe will still be able to move, and most patients will not notice a change in the way they walk or run.
Ostectomy (Haglunds)
Occasionally there may be a spur or bony protrusion from the heel causing injury to the achilles tendon. As part of the tendon debridement and repair procedure, this bony spur may also be excised. Repair of the tendon in these instances may require the use of metal or plastic anchors to help hold the Achilles tendon to the heel bone, where it attaches.
Gastrocnemius Recession
Gastrocnemius Recession involve the surgical lengthening of the calf (gastrocnemius) muscles. Tight calf muscles can cause a wide range of problems including foot and ankle pain, and can place increased stress on the Achilles tendon. This type of surgery may be beneficial depending on your underlying pathology.
Achilles Tendon Surgery Procedure Steps
Surgical objectives include:
- Stitching the torn tendon back together with strong sutures,
- Reinforce the Achilles Tendon with other tendons depending on the extent of the tears
- Where the tendon has avulsed or pulled off the heel bone, the tendon is reattached to the heel bone.
- If the tendon is short, then lengthening may be done
- The tendon attachment to the heel bone will be strengthened with sutures.
The procedure is performed after appropriate diagnostic assessments, pre surgery checks and preparations are complete.
The procedure is normally performed under a general anaesthetic can includes the following steps:
- An incision is then made in your calf muscle to allow the surgeon access to the sheath that surrounds the tendon
- Repair any rips in the tendon using sutures
- Remove the degenerated or damaged portions of the tendon and any bone which is irritating the tendon
- Where required the tendon attachment to the heel bone will be strengthened with sutures.
- At the end the surgery the incision is closed and the patient is sent to the recovery ward for observation
Achilles Tendon Surgery Preparation
Once you and your surgeon have decided that surgery is required, preparation is necessary to achieve the best results and a quick and problem free recovery.
- Infections - Treat any tooth, gum, bladder or bowel problems before surgery to reduce the risk of infection
- Smoking - Stop or cut down smoking to reduce your surgery risks and improve your recovery
- Weight - Consider losing weight (if overweight) before surgery
- Medications - refer Medication Information below
- Fast beforehand - Depending on the type of anaesthesia you'll be receiving, your doctor may advise you to refrain from eating and drinking six to twelve hours before the procedure.
- Arrange for a ride - You will not be allowed to drive yourself home after the procedure, so make arrangements for someone to pick you up. If you live alone, arrange for someone to check on you that evening or, ideally, to stay with you for the rest of the day.
Returning Home After Surgery
When you go home you need to take special precautions around the house to make sure it is safe. Your post operative plans should include:
- Mobility or Stability - You may have to accommodate crutches, wheelchair or knee scooter and may need ramps for stairs
- Sleeping - modify your sleeping arrangements (especially if you are sleeping upstairs) for easy access
- Access - ensure you have easy access to food, water, medications and any other essentials
- Showering - You may require rails in your bathroom or a shower chair, and will and a specialised shower bag to keep your foot dry
Assess your home situation to ensure you have adequate home support in the first few weeks following surgery. If you live alone it may be necessary to arrange a package of community care to help during the first few weeks at home.
Achilles Tendon Surgery Process
Achilles Tendon Rehabilitation Program
Achilles Tendon Risks & Complications Associated
Surgical Follow Ups
How Can I Minimise Post Operative Complications?
- Elevation - Keeping your foot/ankle elevated above your heart when sitting and sleeping will help with pain, swelling and help wound healing
- Blood clots (DVT or PE) - Through early mobilisation, stockings, and medications
- Pain - Keep on top of pain with regular use of pain medications as directed by your surgeon
- Dressings - Keep dressings dry and intact
- Shoewear / Cast- Keep your prescribed shoe (heel wedge, moonboot) on as instructed
- Let us know early if you have any questions or worries
What Are the Consequences of Surgery?
Sometimes the potential risks and consequences of your surgical procedure need to be weighed against the benefits of a successful surgical outcome.
These benefits can include:
- Freedom from pain
- Increased movement
- Greater flexibility
- Maintained independence
- Improved outlook
- Longer more enjoyable life