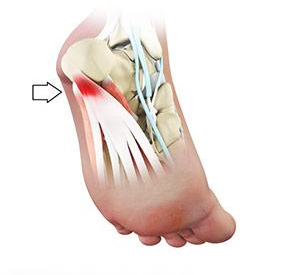
Plantar Fasciitis
What is Plantar Fasciitis?
Plantar Fasciitis is a common and uncomfortable problem that causes heel pain.
Plantar Fasciitis refers to inflammation of the plantar fascia, a thick band of tissue that lies at the bottom of the foot. It runs from the heel bone to the toe and forms the arch of your foot.
Who Does Plantar Fasciitis Affect?
It is most often seen in middle-aged men and women, but may also occur in those who are constantly on their feet.
Cause of Plantar Fasciitis
The plantar fascia functions as a shock absorber and supports the arch of your foot. Excessive pressure over the fascia may strain and tear the tissue causing heel pain.
Repeated overstretching or overuse causes irritation or inflammation of the fascia.
Other risk factors may include
- Obesity
- Foot arch problems such as flat feet or high arches
- Activities such as long-distance running
- Ballet and dance aerobics
- Occupations that necessitate walking or standing on hard surfaces for a long period
- Wearing shoes with poor arch support or thin-soled shoes
Symptoms of Plantar Fasciitis
The most common symptom is stabbing pain on the bottom of the foot near the heel. Pain is experienced when you take your first steps on awakening and it slowly decreases, but may return after standing or walking for long periods.
Diagnosis of Plantar Fasciitis
Patients who suspect they have sustained Plantar Fasciitis should seek a medical consultation. The diagnosis for a Plantar Fasciitis can often include:
Medical History
Your doctor will ask questions about:
- Current symptoms and their severity
- If an injury was sustained
- Your medical history including family or genetic links
- Your current and past medications
- The impact of the problem on your occupation and lifestyle
Physical Examination
Your doctor perform comprehensive physical evaluation that will include:
- Examining the affected area for swelling, pain, bruising or other features
- Assessing your range of motion, walking pattern and other relevant features
Diagnostic Testing
Once your doctor has completed the physical examination further tests maybe required. These tests can help your doctor determine or eliminate possible causes. These can include:
- X-Ray
- Ultrasound (US)
- Computerised Tomography (CT)
- Magnetic Resonance Imaging (MRI)
Once a final diagnosis has been completed your doctor can discuss with you and recommend any treatment options.
Treatment of Plantar Fasciitis
Most patients with plantar fasciitis are effectively treated using a multi-faceted approach possibly including the following measures:
- Rest: Resting the affected area or pausing athletic activity until the symptoms have faded
- Pain medication: Paracetamol, Ibuprofen or Nonsteroidal anti-inflammatory medications (NSAIDs) can relieve some pain or discomfort
- Night Splints: Night splints stretch the plantar fascia and can allow it to heal
- Physiotherapy: Your physiotherapist may design an exercise program that focuses on stretching your plantar fascia and Achilles tendon, and strengthening the muscles of the lower leg.
- Taping: Application of athletic taping to support the bottom of your foot may also help relieve symptoms.
- Extracorporeal Shock Wave Therapy: Also known as ECSW, Shockwave Therapy delivers targeting sound impulses into the plantar fascia. This may help stimulate the healing process for damaged tissues.
- Shoe wear modification: You may require accomodative or custom shoewear to help support your foot.
- Orthotics: Special shoe inserts (heel inserts) may also be prescribed to help relieve the pain.
- Injection Therapies: In more advanced cases of plantar fascitis, a corticosteroid injection can help to to reduce inflammation and pain.
Surgery for Plantar Fasciitis
Surgery is an option for plantar fasciitis but is highly unpredictable and is therefore only used in severe cases that fail to improve with non-operative measures. This involves releasing a small portion of Plantar Fascia when the fascia becomes tightened or is contracted to cause inflammation and pain.